Pathophysiology of wound healing pdf
Wound healing can be delayed by systemic factors that bear little or no direct relation to the location of the wound itself. These include age, body type, chronic disease, immunosuppression, nutritional status, radiation therapy, and vascular insufficiencies.
Granulation. The proliferative phase of wound healing is characterised by granulation, contraction and epithelialisation (Flanagan, 1998a). Granulation tissue, which was first identified by John Hunter in 1786 (Dealey, 1999), is composed of a newly formed wound matrix, consisting of collagen, matrix proteins and proteoglycans (Daly, 1990).
Burn injuries represent a specific wound entity with unique clinical features which range from the difficulty of initial assessment to the long-term tendency to develop pathologic scars. For long time considered as acute wounds, burns are in fact wounds showing a long term evolution transforming
The use of human skin equivalents has been shown to promote wound healing in diabetic ulcers via the action of cytokines and dermal matrix components that stimulate tissue growth and wound closure. 34,35 A recombinant platelet-derived growth factor is also currently in use and has been shown to stimulate wound healing. 36 However, the present data for most of these modalities are not
Wound-healing model. After 1 week of diabetes induction, the normal and After 1 week of diabetes induction, the normal and diabetic rats were used for wound-healing studies.
The literature that exists on the subject of wound healing and tissue repair is vast, and it is soon apparent to anyone who begins to survey it that the majority of studies have been carried out on skin. This of course is not surprising in view of its ready accessibility for experiment and …
the pathophysiology of chronic wounds and rationale for wound bed preparation with negative-pressure therapy dr.ehren eksteen , prof pf coetzee
Clinical Practice Guidelines. In 2003, the Wound Healing Foundation (WHF) and president Dr. Elof Eriksson determined that standards based on evidence should be developed specific for wound healing.
Impaired wound healing is a frequent and very severe problem in patients with diabetes mellitus, yet little is known about the underlying pathomechanisms. In this paper we review the biology of wound healing with particular attention to the pathophysiology of chronic wounds in diabetic patients. The standard treatment of diabetic ulcers
A bone fracture (sometimes abbreviated FRX or Fx, F x, or #) is a medical condition in which there is a partial or complete break in the continuity of the bone. In more severe cases, the bone may be broken into several pieces. [1]
Physiology of wound healing Advanced wound assessment Advanced wound dressing products Wound debridement o Theoretical o Practical Wound infection Complex wound types (leg ulcers, pressure ulcers, diabetic foot ulcers, malignant/fungating tumours) Vascular assessment o Theoretical o Practical Compression bandaging o Theoretical o Practical Complex case studies – 7 – Advanced Wound …
A reliable method of determining wound healing rate D. Cukjati S. Rebersˇek D. Miklavcˇicˇ Faculty of Electrical Engineering, University of Ljubljana, Ljubljana, Slovenia Abstract—Several wound healing rate measures have been introduced with the main goal of enabling quantification of the effects of various therapeutic modalities on the healing of open wounds. Different definitions of
Wound classification and the basic principles of wound healing are reviewed here. The factors responsible for impaired wound healing and wound complications, as well as the clinical assessment and management of wounds, are reviewed elsewhere. (See
pdf PDF Plus There has been a great deal of research into the ways in which drugs affect the physiology of wound healing, but to understand it the nurse must know what the normal processes are.
Burn Pathophysiology Vic Burns
https://youtube.com/watch?v=j4v7PFw5wA0
(PDF) PATHOPHYSIOLOGY OF WOUND HEALING
Clinics in Dermatology (2007) 25, 9 – 18. Pathophysiology of acute wound healing Jie Li, PhD*, Juan Chen, MD, Robert Kirsner, PhD Department of Dermatology and Cutaneous Surgery, University of Miami Miller School of Medicine, Miami, FL 33136, USA
Diabetic foot ulcer is a major complication of diabetes mellitus, and probably the major component of the diabetic foot. Wound healing is an innate mechanism of action that works reliably most of the time.
Annals of Burns and Fire Disasters – vol. XVII – n. 3 – September 2004 Introduction Research on burn wound pathophysiology has evolved fast in the last decade, especially as regards
Burn Pathophysiology Jackson’s Burn Wound Model is a model for understanding the pathophysiology of a burn wound that has been often described in the literature( 4-10 ). The zone of coagulation nearest the heat source is the primary injury.
This review will cover some important aspects of general wound healing, and then discuss the important aspect of the pathophysiology of wound healing in VLU, differentiate VLU that heal versus VLU that are classified as non-healing with respect to the biochemical properties of the wound.
Venous leg ulcer (VLU) is one of the most common lower extremity ulcerated wound, and is a significant healthcare problem with implications that affect social, economic, and the well-being of a patient. VLU can have debilitating related problems which require weekly medical care and may take months to years to heal. The pathophysiology of VLU
Wound healing is a complex process of repairing after tissue injury. Burn is one of the most common types of injuries. SSD cream is the gold standard treatment used for preventing bacterial gram positive and gram negative growth in the burn wound and for wound healing.
Storch, J. E. and Rice, J. (2005) Clinical Issues in the Causes of Wound Breakdown and the Failure of Wounds to Repair, in Reconstructive Plastic Surgical Nursing: Clinical Management and Wound Care, Blackwell Publishing Ltd, Oxford, UK. doi: 10.1002/9780470774656.ch8
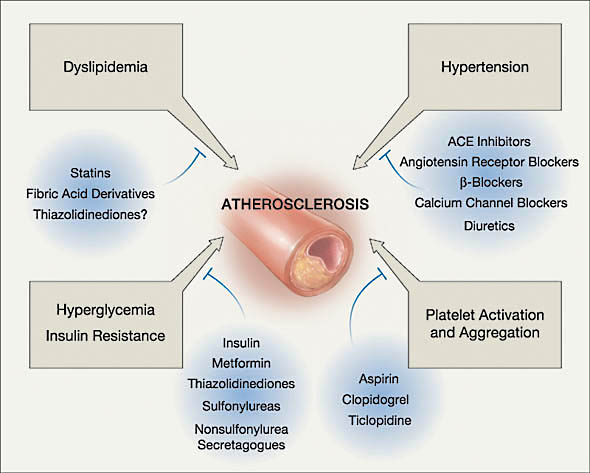
inflammation and wound healing. 25.Systemic reactions in inflammation Mechanism of the development of fever, fever patterns. The biological significance of fever. Role of leukocytosis and thrombocyte aggregation. Alterations in the synthesis of serum proteins. Acute phase proteins. 26.Evolution of atherosclerosis – lipid theory of atherosclerosis Process of the development of …
Pathophysiology of wound healing Normal wound healing involves a complex and dynamic but superbly orchestrated series of events leading to the repair of …
Albumin is a protein responsible for wo und healing; a decrease will cause a delay in the pro cess of wound healing. Due to hypoalbuminea, a disruption in the anastomosis and leaking happens as evidence by yellowish abdominal secretions that lead to tertiary peritonitis. Tertiary peritonitis is an inflammation of the peritoneum after a surgical procedure to control secondary peritonitis. It
Impaired wound healing is not an uncommon occurrence in clinical practice. Both local and systemic factors are responsible for impaired healing and weak scar tissue formation. Acute wounds heal following the normal sequence of the healing process.
• Review the physiology and pathophysiology of wound healing in diabetes • Summarize keys to the diagnostic workup for patients with diabetic foot ulcers • Examine the role of growth factor therapy as an evidence-based biologic therapy for treating diabetic foot ulcers

Wound healing is an evolutionary conserved process that aims to restore the damaged barrier. This complex process involves many cellular responses including inflammation, proliferation, migration, angiogenesis, and tissue remodeling.
ABSTRACT: This is the second of 2 articles that discuss the biology and pathophysiology of wound healing, reviewing the role that growth factors play in this process and describing the current methods for growth factor delivery into the wound bed
Wound healing and diabetes mellitus David G. Greenhalgh, MDa,b,* aShriners Hospitals for Children Northern California, 2425 Stockton Boulevard, Sacramento, CA 95817, USA bDepartment of Surgery, University of California at Davis, 2730 Stockton Boulevard, Sacramento, CA 95817, USA One of the leading causes of impaired wound healing is diabetes mellitus. Unlike other causes of altered tissue
• A review of 32 abdominal wound dehiscences in a five-year period shows an incidence of 0.51%. Important factors are preexisting pulmonary disease, “malnutrition,” intraoperative contamination (often minimal), gastrointestinal distention, and aggressive tracheobronchial toilet in the postoperative period.
Abstract. Wound healing is a complex process that can be divided into at least 3 continuous and overlapping processes: an inflammatory reaction, a proliferative process leading to tissue restoration, and, eventually, tissue remodeling.
Review the physiology and pathophysiology of wound healing in diabetes Summarize keys to the diagnostic workup for patients with diabetic foot ulcers Examine the role of growth factor therapy as an evidence-based biologic therapy for treating diabetic foot ulcers
Wound healing is a complex and highly regulated process that can be compromised by both endogenous factors (pathophysiological) and exogenous factors (micro-organisms). Microbial colonisation of both acute and chronic wounds is inevitable, and in most situations endogenous bacteria predominate, many
PHYSIOLOGY OF HEALING. The healing process is divided into three broad stages which are not mutually exclusive and overlap considerably. 1.Initial vascular reaction 2.Inflammatory response 3. Proliferative phase 4. Remodeling Wound healing refers to the body’s replacement of destroyed tissue by living tissue (Walter & Israel 1987). It comprises of two essential components whose
Wound care is “the provision of the appropriate environment for healing by both direct and indirect 1methods together with the prevention of skin breakdown”. In
https://youtube.com/watch?v=j4v7PFw5wA0
Pathophysiology of Wound Healing ScienceDirect
Pathophysiology of Morbid Obesity Tony Burn Alfred Hospital, Melbourne, Australia Introduction Obesity is an epidemic disease which is increasing in frequency in Australia
Diabetes Pathophysiology. Download PDF Copy; By Ananya Mandal, MD Reviewed by April Cashin-Garbutt, MA (Cantab) Diabetes occurs when there is a dis …
The initiation of healing starts with the creation of a wound. A wound is defined as an injury to the body that typically involves laceration or breaking of a membrane and damage to the underlying tissues.1 Injury can occur from any number of mechanical or thermal forces that lead to disruption of the skin and damage to the connective tissue and vasculature. Bleeding ensues along with exposure
pathophysiology of burns . Major thermal injuries are accompanied by marked pathophysiological and immunological changes. These have been extensively detailed by Arturson (1985 pp.129-146) and Britto et al (1999 pp.103-112).
After cutaneous injury, the pathophysiology of wound healing is characterized by an inflammatory phase (days 1-3), a proliferative phase (days 4-21), and a remodeling phase (day 21 to year 1). Mammalian cutaneous wounds during the first third of gestation do not scar, because healing occurs via tissue regenerative pathways.
Pathophysiology of Wound Healing Christopher M Halloran John P Slavin Christopher M Halloran is a Specialist Registrar/Research Fellow at the Department of Surgery, Royal Liverpool University Hospital, UK. He qualified from Liverpool University. His main research interest is the use of gene therapy as an adjunct in pancreatic cancer treatment. John P Slavin is a Senior Lecturer in the
This is the first installment of 2 articles that discuss the biology and pathophysiology of wound healing, review the role that growth factors play in this process, and describe current ways of growth factor delivery into the wound bed.
Recent Advances: Although often difficult to treat, an understanding of the underlying pathophysiology and specific attention toward managing these perturbations can often lead to successful healing. Critical Issues: Overcoming the factors that contribute to delayed healing are key components of a comprehensive approach to wound care and present the primary challenges to the treatment of
WHS Guidelines The Wound Healing Foundation
HISTORY OF WOUND HEALING • Wood Johnson(1876): – Antiseptic dressing (cotton gauze impregnated with iodoform). • The 1960s and 1970s: – Developing of polymeric dressing
The mechanisms of wound healing in general have gained interest in recent years, as it has become obvious that the tightly regulated process of tissue repair and regeneration is of great importance for organ homeostasis.
How Diabetes Affects Wound Healing. Tweet. Diabetes is a condition in which the body does not effectively use sugar. It is estimated that there are nearly 18 million Americans with diabetes, and approximately 15 percent of diabetics will develop a foot ulcer at some point. Foot ulcers are the most common wounds for this patient population. Wound healing can be slowed when the patient is
Pathophysiology of wound healing and alterations in venous
Oxygen and wound healing Pathophysiology
https://youtube.com/watch?v=20HX4BFxBRQ
Pathophysiology of acute wound healing ScienceDirect
Physiology and Pathophysiology of Wound Healing in
Diabetic foot ulcer Wikipedia

Pathophysiology of Peptic Ulcer Proceedings of the Second
Regulation of wound healing Pathophysiology
Wound healing and diabetes mellitus Semantic Scholar

Pathophysiology of Wound Healing Wound Healing Scribd
Burn Wound Healing Pathophysiology and Current Management
Pathophysiology of wound healing and alterations in venous
Oxygen and wound healing Pathophysiology
Clinics in Dermatology (2007) 25, 9 – 18. Pathophysiology of acute wound healing Jie Li, PhD*, Juan Chen, MD, Robert Kirsner, PhD Department of Dermatology and Cutaneous Surgery, University of Miami Miller School of Medicine, Miami, FL 33136, USA
Wound care is “the provision of the appropriate environment for healing by both direct and indirect 1methods together with the prevention of skin breakdown”. In
the pathophysiology of chronic wounds and rationale for wound bed preparation with negative-pressure therapy dr.ehren eksteen , prof pf coetzee
pathophysiology of burns . Major thermal injuries are accompanied by marked pathophysiological and immunological changes. These have been extensively detailed by Arturson (1985 pp.129-146) and Britto et al (1999 pp.103-112).
PHYSIOLOGY OF HEALING. The healing process is divided into three broad stages which are not mutually exclusive and overlap considerably. 1.Initial vascular reaction 2.Inflammatory response 3. Proliferative phase 4. Remodeling Wound healing refers to the body’s replacement of destroyed tissue by living tissue (Walter & Israel 1987). It comprises of two essential components whose
A bone fracture (sometimes abbreviated FRX or Fx, F x, or #) is a medical condition in which there is a partial or complete break in the continuity of the bone. In more severe cases, the bone may be broken into several pieces. [1]
The literature that exists on the subject of wound healing and tissue repair is vast, and it is soon apparent to anyone who begins to survey it that the majority of studies have been carried out on skin. This of course is not surprising in view of its ready accessibility for experiment and …
How Diabetes Affects Wound Healing WoundCareCenters.org
Pathophysiology of wound healing and alterations in venous
Wound-healing model. After 1 week of diabetes induction, the normal and After 1 week of diabetes induction, the normal and diabetic rats were used for wound-healing studies.
Pathophysiology of Wound Healing Christopher M Halloran John P Slavin Christopher M Halloran is a Specialist Registrar/Research Fellow at the Department of Surgery, Royal Liverpool University Hospital, UK. He qualified from Liverpool University. His main research interest is the use of gene therapy as an adjunct in pancreatic cancer treatment. John P Slavin is a Senior Lecturer in the
Wound healing and diabetes mellitus David G. Greenhalgh, MDa,b,* aShriners Hospitals for Children Northern California, 2425 Stockton Boulevard, Sacramento, CA 95817, USA bDepartment of Surgery, University of California at Davis, 2730 Stockton Boulevard, Sacramento, CA 95817, USA One of the leading causes of impaired wound healing is diabetes mellitus. Unlike other causes of altered tissue
Impaired wound healing is a frequent and very severe problem in patients with diabetes mellitus, yet little is known about the underlying pathomechanisms. In this paper we review the biology of wound healing with particular attention to the pathophysiology of chronic wounds in diabetic patients. The standard treatment of diabetic ulcers
Wound classification and the basic principles of wound healing are reviewed here. The factors responsible for impaired wound healing and wound complications, as well as the clinical assessment and management of wounds, are reviewed elsewhere. (See
pathophysiology of burns . Major thermal injuries are accompanied by marked pathophysiological and immunological changes. These have been extensively detailed by Arturson (1985 pp.129-146) and Britto et al (1999 pp.103-112).
Physiology of wound healing Advanced wound assessment Advanced wound dressing products Wound debridement o Theoretical o Practical Wound infection Complex wound types (leg ulcers, pressure ulcers, diabetic foot ulcers, malignant/fungating tumours) Vascular assessment o Theoretical o Practical Compression bandaging o Theoretical o Practical Complex case studies – 7 – Advanced Wound …
Wound healing is a complex and highly regulated process that can be compromised by both endogenous factors (pathophysiological) and exogenous factors (micro-organisms). Microbial colonisation of both acute and chronic wounds is inevitable, and in most situations endogenous bacteria predominate, many
Abstract. Wound healing is a complex process that can be divided into at least 3 continuous and overlapping processes: an inflammatory reaction, a proliferative process leading to tissue restoration, and, eventually, tissue remodeling.
After cutaneous injury, the pathophysiology of wound healing is characterized by an inflammatory phase (days 1-3), a proliferative phase (days 4-21), and a remodeling phase (day 21 to year 1). Mammalian cutaneous wounds during the first third of gestation do not scar, because healing occurs via tissue regenerative pathways.
Pathophysiology of Wound Healing Wound Healing Scribd
Pathophysiology of Peptic Ulcer Proceedings of the Second
Recent Advances: Although often difficult to treat, an understanding of the underlying pathophysiology and specific attention toward managing these perturbations can often lead to successful healing. Critical Issues: Overcoming the factors that contribute to delayed healing are key components of a comprehensive approach to wound care and present the primary challenges to the treatment of
Granulation. The proliferative phase of wound healing is characterised by granulation, contraction and epithelialisation (Flanagan, 1998a). Granulation tissue, which was first identified by John Hunter in 1786 (Dealey, 1999), is composed of a newly formed wound matrix, consisting of collagen, matrix proteins and proteoglycans (Daly, 1990).
Impaired wound healing is a frequent and very severe problem in patients with diabetes mellitus, yet little is known about the underlying pathomechanisms. In this paper we review the biology of wound healing with particular attention to the pathophysiology of chronic wounds in diabetic patients. The standard treatment of diabetic ulcers
Pathophysiology of Wound Healing Christopher M Halloran John P Slavin Christopher M Halloran is a Specialist Registrar/Research Fellow at the Department of Surgery, Royal Liverpool University Hospital, UK. He qualified from Liverpool University. His main research interest is the use of gene therapy as an adjunct in pancreatic cancer treatment. John P Slavin is a Senior Lecturer in the
Wound healing is a complex and highly regulated process that can be compromised by both endogenous factors (pathophysiological) and exogenous factors (micro-organisms). Microbial colonisation of both acute and chronic wounds is inevitable, and in most situations endogenous bacteria predominate, many
Burn Pathophysiology Jackson’s Burn Wound Model is a model for understanding the pathophysiology of a burn wound that has been often described in the literature( 4-10 ). The zone of coagulation nearest the heat source is the primary injury.
Abstract. Wound healing is a complex process that can be divided into at least 3 continuous and overlapping processes: an inflammatory reaction, a proliferative process leading to tissue restoration, and, eventually, tissue remodeling.
Pathophysiology of Peptic Ulcer Proceedings of the Second
Pathophysiology of Morbid Obesity Conference Innovators
• A review of 32 abdominal wound dehiscences in a five-year period shows an incidence of 0.51%. Important factors are preexisting pulmonary disease, “malnutrition,” intraoperative contamination (often minimal), gastrointestinal distention, and aggressive tracheobronchial toilet in the postoperative period.
Albumin is a protein responsible for wo und healing; a decrease will cause a delay in the pro cess of wound healing. Due to hypoalbuminea, a disruption in the anastomosis and leaking happens as evidence by yellowish abdominal secretions that lead to tertiary peritonitis. Tertiary peritonitis is an inflammation of the peritoneum after a surgical procedure to control secondary peritonitis. It
Wound healing is an evolutionary conserved process that aims to restore the damaged barrier. This complex process involves many cellular responses including inflammation, proliferation, migration, angiogenesis, and tissue remodeling.
Granulation. The proliferative phase of wound healing is characterised by granulation, contraction and epithelialisation (Flanagan, 1998a). Granulation tissue, which was first identified by John Hunter in 1786 (Dealey, 1999), is composed of a newly formed wound matrix, consisting of collagen, matrix proteins and proteoglycans (Daly, 1990).
Wound healing is a complex and highly regulated process that can be compromised by both endogenous factors (pathophysiological) and exogenous factors (micro-organisms). Microbial colonisation of both acute and chronic wounds is inevitable, and in most situations endogenous bacteria predominate, many
The initiation of healing starts with the creation of a wound. A wound is defined as an injury to the body that typically involves laceration or breaking of a membrane and damage to the underlying tissues.1 Injury can occur from any number of mechanical or thermal forces that lead to disruption of the skin and damage to the connective tissue and vasculature. Bleeding ensues along with exposure
Clinical Issues in the Causes of Wound Breakdown and the
Assessment of the histological state of the healing wound
Wound healing is a complex and highly regulated process that can be compromised by both endogenous factors (pathophysiological) and exogenous factors (micro-organisms). Microbial colonisation of both acute and chronic wounds is inevitable, and in most situations endogenous bacteria predominate, many
Clinics in Dermatology (2007) 25, 9 – 18. Pathophysiology of acute wound healing Jie Li, PhD*, Juan Chen, MD, Robert Kirsner, PhD Department of Dermatology and Cutaneous Surgery, University of Miami Miller School of Medicine, Miami, FL 33136, USA
Burn injuries represent a specific wound entity with unique clinical features which range from the difficulty of initial assessment to the long-term tendency to develop pathologic scars. For long time considered as acute wounds, burns are in fact wounds showing a long term evolution transforming
This review will cover some important aspects of general wound healing, and then discuss the important aspect of the pathophysiology of wound healing in VLU, differentiate VLU that heal versus VLU that are classified as non-healing with respect to the biochemical properties of the wound.
Pathophysiology of Morbid Obesity Tony Burn Alfred Hospital, Melbourne, Australia Introduction Obesity is an epidemic disease which is increasing in frequency in Australia
Wound healing and diabetes mellitus David G. Greenhalgh, MDa,b,* aShriners Hospitals for Children Northern California, 2425 Stockton Boulevard, Sacramento, CA 95817, USA bDepartment of Surgery, University of California at Davis, 2730 Stockton Boulevard, Sacramento, CA 95817, USA One of the leading causes of impaired wound healing is diabetes mellitus. Unlike other causes of altered tissue
ABSTRACT: This is the second of 2 articles that discuss the biology and pathophysiology of wound healing, reviewing the role that growth factors play in this process and describing the current methods for growth factor delivery into the wound bed
After cutaneous injury, the pathophysiology of wound healing is characterized by an inflammatory phase (days 1-3), a proliferative phase (days 4-21), and a remodeling phase (day 21 to year 1). Mammalian cutaneous wounds during the first third of gestation do not scar, because healing occurs via tissue regenerative pathways.
Abstract. Wound healing is a complex process that can be divided into at least 3 continuous and overlapping processes: an inflammatory reaction, a proliferative process leading to tissue restoration, and, eventually, tissue remodeling.
Impaired wound healing is a frequent and very severe problem in patients with diabetes mellitus, yet little is known about the underlying pathomechanisms. In this paper we review the biology of wound healing with particular attention to the pathophysiology of chronic wounds in diabetic patients. The standard treatment of diabetic ulcers
The literature that exists on the subject of wound healing and tissue repair is vast, and it is soon apparent to anyone who begins to survey it that the majority of studies have been carried out on skin. This of course is not surprising in view of its ready accessibility for experiment and …
Clinical Issues in the Causes of Wound Breakdown and the
Pathophysiology of Wound Healing ScienceDirect
HISTORY OF WOUND HEALING • Wood Johnson(1876): – Antiseptic dressing (cotton gauze impregnated with iodoform). • The 1960s and 1970s: – Developing of polymeric dressing
Diabetic foot ulcer is a major complication of diabetes mellitus, and probably the major component of the diabetic foot. Wound healing is an innate mechanism of action that works reliably most of the time.
ABSTRACT: This is the second of 2 articles that discuss the biology and pathophysiology of wound healing, reviewing the role that growth factors play in this process and describing the current methods for growth factor delivery into the wound bed
Burn Pathophysiology Jackson’s Burn Wound Model is a model for understanding the pathophysiology of a burn wound that has been often described in the literature( 4-10 ). The zone of coagulation nearest the heat source is the primary injury.
Impaired wound healing is a frequent and very severe problem in patients with diabetes mellitus, yet little is known about the underlying pathomechanisms. In this paper we review the biology of wound healing with particular attention to the pathophysiology of chronic wounds in diabetic patients. The standard treatment of diabetic ulcers
Review the physiology and pathophysiology of wound healing in diabetes Summarize keys to the diagnostic workup for patients with diabetic foot ulcers Examine the role of growth factor therapy as an evidence-based biologic therapy for treating diabetic foot ulcers
Impaired wound healing is not an uncommon occurrence in clinical practice. Both local and systemic factors are responsible for impaired healing and weak scar tissue formation. Acute wounds heal following the normal sequence of the healing process.
Pathophysiology of wound healing Normal wound healing involves a complex and dynamic but superbly orchestrated series of events leading to the repair of …
Physiology of wound healing Advanced wound assessment Advanced wound dressing products Wound debridement o Theoretical o Practical Wound infection Complex wound types (leg ulcers, pressure ulcers, diabetic foot ulcers, malignant/fungating tumours) Vascular assessment o Theoretical o Practical Compression bandaging o Theoretical o Practical Complex case studies – 7 – Advanced Wound …
This review will cover some important aspects of general wound healing, and then discuss the important aspect of the pathophysiology of wound healing in VLU, differentiate VLU that heal versus VLU that are classified as non-healing with respect to the biochemical properties of the wound.
Pathophysiology of Wound Healing Wound Healing Scribd
Medication and wound healing Practice Nursing Vol 9 No 14
This is the first installment of 2 articles that discuss the biology and pathophysiology of wound healing, review the role that growth factors play in this process, and describe current ways of growth factor delivery into the wound bed.
The initiation of healing starts with the creation of a wound. A wound is defined as an injury to the body that typically involves laceration or breaking of a membrane and damage to the underlying tissues.1 Injury can occur from any number of mechanical or thermal forces that lead to disruption of the skin and damage to the connective tissue and vasculature. Bleeding ensues along with exposure
Impaired wound healing is not an uncommon occurrence in clinical practice. Both local and systemic factors are responsible for impaired healing and weak scar tissue formation. Acute wounds heal following the normal sequence of the healing process.
• A review of 32 abdominal wound dehiscences in a five-year period shows an incidence of 0.51%. Important factors are preexisting pulmonary disease, “malnutrition,” intraoperative contamination (often minimal), gastrointestinal distention, and aggressive tracheobronchial toilet in the postoperative period.
Pathophysiology exam questions Semmelweis Egyetem
Regulation of wound healing Pathophysiology
Venous leg ulcer (VLU) is one of the most common lower extremity ulcerated wound, and is a significant healthcare problem with implications that affect social, economic, and the well-being of a patient. VLU can have debilitating related problems which require weekly medical care and may take months to years to heal. The pathophysiology of VLU
the pathophysiology of chronic wounds and rationale for wound bed preparation with negative-pressure therapy dr.ehren eksteen , prof pf coetzee
PHYSIOLOGY OF HEALING. The healing process is divided into three broad stages which are not mutually exclusive and overlap considerably. 1.Initial vascular reaction 2.Inflammatory response 3. Proliferative phase 4. Remodeling Wound healing refers to the body’s replacement of destroyed tissue by living tissue (Walter & Israel 1987). It comprises of two essential components whose
Wound classification and the basic principles of wound healing are reviewed here. The factors responsible for impaired wound healing and wound complications, as well as the clinical assessment and management of wounds, are reviewed elsewhere. (See
A reliable method of determining wound healing rate D. Cukjati S. Rebersˇek D. Miklavcˇicˇ Faculty of Electrical Engineering, University of Ljubljana, Ljubljana, Slovenia Abstract—Several wound healing rate measures have been introduced with the main goal of enabling quantification of the effects of various therapeutic modalities on the healing of open wounds. Different definitions of
Annals of Burns and Fire Disasters – vol. XVII – n. 3 – September 2004 Introduction Research on burn wound pathophysiology has evolved fast in the last decade, especially as regards
• Review the physiology and pathophysiology of wound healing in diabetes • Summarize keys to the diagnostic workup for patients with diabetic foot ulcers • Examine the role of growth factor therapy as an evidence-based biologic therapy for treating diabetic foot ulcers
Wound healing and diabetes mellitus David G. Greenhalgh, MDa,b,* aShriners Hospitals for Children Northern California, 2425 Stockton Boulevard, Sacramento, CA 95817, USA bDepartment of Surgery, University of California at Davis, 2730 Stockton Boulevard, Sacramento, CA 95817, USA One of the leading causes of impaired wound healing is diabetes mellitus. Unlike other causes of altered tissue
Medication and wound healing Practice Nursing Vol 9 No 14
ORIGINAL ARTICLE High-Glucose Environment Enhanced
ABSTRACT: This is the second of 2 articles that discuss the biology and pathophysiology of wound healing, reviewing the role that growth factors play in this process and describing the current methods for growth factor delivery into the wound bed
Wound healing and diabetes mellitus David G. Greenhalgh, MDa,b,* aShriners Hospitals for Children Northern California, 2425 Stockton Boulevard, Sacramento, CA 95817, USA bDepartment of Surgery, University of California at Davis, 2730 Stockton Boulevard, Sacramento, CA 95817, USA One of the leading causes of impaired wound healing is diabetes mellitus. Unlike other causes of altered tissue
Wound classification and the basic principles of wound healing are reviewed here. The factors responsible for impaired wound healing and wound complications, as well as the clinical assessment and management of wounds, are reviewed elsewhere. (See
Recent Advances: Although often difficult to treat, an understanding of the underlying pathophysiology and specific attention toward managing these perturbations can often lead to successful healing. Critical Issues: Overcoming the factors that contribute to delayed healing are key components of a comprehensive approach to wound care and present the primary challenges to the treatment of
• Review the physiology and pathophysiology of wound healing in diabetes • Summarize keys to the diagnostic workup for patients with diabetic foot ulcers • Examine the role of growth factor therapy as an evidence-based biologic therapy for treating diabetic foot ulcers
Annals of Burns and Fire Disasters – vol. XVII – n. 3 – September 2004 Introduction Research on burn wound pathophysiology has evolved fast in the last decade, especially as regards
Physiology of wound healing Advanced wound assessment Advanced wound dressing products Wound debridement o Theoretical o Practical Wound infection Complex wound types (leg ulcers, pressure ulcers, diabetic foot ulcers, malignant/fungating tumours) Vascular assessment o Theoretical o Practical Compression bandaging o Theoretical o Practical Complex case studies – 7 – Advanced Wound …
Impaired wound healing is not an uncommon occurrence in clinical practice. Both local and systemic factors are responsible for impaired healing and weak scar tissue formation. Acute wounds heal following the normal sequence of the healing process.
Wound-healing model. After 1 week of diabetes induction, the normal and After 1 week of diabetes induction, the normal and diabetic rats were used for wound-healing studies.
PHYSIOLOGY OF HEALING. The healing process is divided into three broad stages which are not mutually exclusive and overlap considerably. 1.Initial vascular reaction 2.Inflammatory response 3. Proliferative phase 4. Remodeling Wound healing refers to the body’s replacement of destroyed tissue by living tissue (Walter & Israel 1987). It comprises of two essential components whose
inflammation and wound healing. 25.Systemic reactions in inflammation Mechanism of the development of fever, fever patterns. The biological significance of fever. Role of leukocytosis and thrombocyte aggregation. Alterations in the synthesis of serum proteins. Acute phase proteins. 26.Evolution of atherosclerosis – lipid theory of atherosclerosis Process of the development of …
A reliable method of determining wound healing rate D. Cukjati S. Rebersˇek D. Miklavcˇicˇ Faculty of Electrical Engineering, University of Ljubljana, Ljubljana, Slovenia Abstract—Several wound healing rate measures have been introduced with the main goal of enabling quantification of the effects of various therapeutic modalities on the healing of open wounds. Different definitions of
The literature that exists on the subject of wound healing and tissue repair is vast, and it is soon apparent to anyone who begins to survey it that the majority of studies have been carried out on skin. This of course is not surprising in view of its ready accessibility for experiment and …
Burn Pathophysiology Jackson’s Burn Wound Model is a model for understanding the pathophysiology of a burn wound that has been often described in the literature( 4-10 ). The zone of coagulation nearest the heat source is the primary injury.
Assessment of the histological state of the healing wound
APPENDICITIS PATHOPHYSIOLOGY PDF Free Download
The literature that exists on the subject of wound healing and tissue repair is vast, and it is soon apparent to anyone who begins to survey it that the majority of studies have been carried out on skin. This of course is not surprising in view of its ready accessibility for experiment and …
Annals of Burns and Fire Disasters – vol. XVII – n. 3 – September 2004 Introduction Research on burn wound pathophysiology has evolved fast in the last decade, especially as regards
HISTORY OF WOUND HEALING • Wood Johnson(1876): – Antiseptic dressing (cotton gauze impregnated with iodoform). • The 1960s and 1970s: – Developing of polymeric dressing
Venous leg ulcer (VLU) is one of the most common lower extremity ulcerated wound, and is a significant healthcare problem with implications that affect social, economic, and the well-being of a patient. VLU can have debilitating related problems which require weekly medical care and may take months to years to heal. The pathophysiology of VLU
pdf PDF Plus There has been a great deal of research into the ways in which drugs affect the physiology of wound healing, but to understand it the nurse must know what the normal processes are.
The mechanisms of wound healing in general have gained interest in recent years, as it has become obvious that the tightly regulated process of tissue repair and regeneration is of great importance for organ homeostasis.
Wound classification and the basic principles of wound healing are reviewed here. The factors responsible for impaired wound healing and wound complications, as well as the clinical assessment and management of wounds, are reviewed elsewhere. (See
the pathophysiology of chronic wounds and rationale for wound bed preparation with negative-pressure therapy dr.ehren eksteen , prof pf coetzee
This is the first installment of 2 articles that discuss the biology and pathophysiology of wound healing, review the role that growth factors play in this process, and describe current ways of growth factor delivery into the wound bed.
• Review the physiology and pathophysiology of wound healing in diabetes • Summarize keys to the diagnostic workup for patients with diabetic foot ulcers • Examine the role of growth factor therapy as an evidence-based biologic therapy for treating diabetic foot ulcers
This review will cover some important aspects of general wound healing, and then discuss the important aspect of the pathophysiology of wound healing in VLU, differentiate VLU that heal versus VLU that are classified as non-healing with respect to the biochemical properties of the wound.
Pathophysiology of Wound Healing Christopher M Halloran John P Slavin Christopher M Halloran is a Specialist Registrar/Research Fellow at the Department of Surgery, Royal Liverpool University Hospital, UK. He qualified from Liverpool University. His main research interest is the use of gene therapy as an adjunct in pancreatic cancer treatment. John P Slavin is a Senior Lecturer in the
Wound pathophysiology infection and therapeutic options
Oxygen and wound healing Pathophysiology
Wound healing is an evolutionary conserved process that aims to restore the damaged barrier. This complex process involves many cellular responses including inflammation, proliferation, migration, angiogenesis, and tissue remodeling.
inflammation and wound healing. 25.Systemic reactions in inflammation Mechanism of the development of fever, fever patterns. The biological significance of fever. Role of leukocytosis and thrombocyte aggregation. Alterations in the synthesis of serum proteins. Acute phase proteins. 26.Evolution of atherosclerosis – lipid theory of atherosclerosis Process of the development of …
Wound care is “the provision of the appropriate environment for healing by both direct and indirect 1methods together with the prevention of skin breakdown”. In
Pathophysiology of Wound Healing Christopher M Halloran John P Slavin Christopher M Halloran is a Specialist Registrar/Research Fellow at the Department of Surgery, Royal Liverpool University Hospital, UK. He qualified from Liverpool University. His main research interest is the use of gene therapy as an adjunct in pancreatic cancer treatment. John P Slavin is a Senior Lecturer in the
Impaired wound healing is a frequent and very severe problem in patients with diabetes mellitus, yet little is known about the underlying pathomechanisms. In this paper we review the biology of wound healing with particular attention to the pathophysiology of chronic wounds in diabetic patients. The standard treatment of diabetic ulcers
Pathophysiology of Morbid Obesity Tony Burn Alfred Hospital, Melbourne, Australia Introduction Obesity is an epidemic disease which is increasing in frequency in Australia
WHS Guidelines The Wound Healing Foundation
NON-INVASIVE ASSESSMENT OF WOUND-HEALING PATHOPHYSIOLOGY
Recent Advances: Although often difficult to treat, an understanding of the underlying pathophysiology and specific attention toward managing these perturbations can often lead to successful healing. Critical Issues: Overcoming the factors that contribute to delayed healing are key components of a comprehensive approach to wound care and present the primary challenges to the treatment of
Diabetic foot ulcer is a major complication of diabetes mellitus, and probably the major component of the diabetic foot. Wound healing is an innate mechanism of action that works reliably most of the time.
Review the physiology and pathophysiology of wound healing in diabetes Summarize keys to the diagnostic workup for patients with diabetic foot ulcers Examine the role of growth factor therapy as an evidence-based biologic therapy for treating diabetic foot ulcers
Storch, J. E. and Rice, J. (2005) Clinical Issues in the Causes of Wound Breakdown and the Failure of Wounds to Repair, in Reconstructive Plastic Surgical Nursing: Clinical Management and Wound Care, Blackwell Publishing Ltd, Oxford, UK. doi: 10.1002/9780470774656.ch8
Wound healing and diabetes mellitus David G. Greenhalgh, MDa,b,* aShriners Hospitals for Children Northern California, 2425 Stockton Boulevard, Sacramento, CA 95817, USA bDepartment of Surgery, University of California at Davis, 2730 Stockton Boulevard, Sacramento, CA 95817, USA One of the leading causes of impaired wound healing is diabetes mellitus. Unlike other causes of altered tissue
Wound healing can be delayed by systemic factors that bear little or no direct relation to the location of the wound itself. These include age, body type, chronic disease, immunosuppression, nutritional status, radiation therapy, and vascular insufficiencies.
After cutaneous injury, the pathophysiology of wound healing is characterized by an inflammatory phase (days 1-3), a proliferative phase (days 4-21), and a remodeling phase (day 21 to year 1). Mammalian cutaneous wounds during the first third of gestation do not scar, because healing occurs via tissue regenerative pathways.
Burn Pathophysiology Jackson’s Burn Wound Model is a model for understanding the pathophysiology of a burn wound that has been often described in the literature( 4-10 ). The zone of coagulation nearest the heat source is the primary injury.
NON-INVASIVE ASSESSMENT OF WOUND-HEALING PATHOPHYSIOLOGY
Wound healing and diabetes mellitus Semantic Scholar
This is the first installment of 2 articles that discuss the biology and pathophysiology of wound healing, review the role that growth factors play in this process, and describe current ways of growth factor delivery into the wound bed.
Granulation. The proliferative phase of wound healing is characterised by granulation, contraction and epithelialisation (Flanagan, 1998a). Granulation tissue, which was first identified by John Hunter in 1786 (Dealey, 1999), is composed of a newly formed wound matrix, consisting of collagen, matrix proteins and proteoglycans (Daly, 1990).
Annals of Burns and Fire Disasters – vol. XVII – n. 3 – September 2004 Introduction Research on burn wound pathophysiology has evolved fast in the last decade, especially as regards
Clinical Practice Guidelines. In 2003, the Wound Healing Foundation (WHF) and president Dr. Elof Eriksson determined that standards based on evidence should be developed specific for wound healing.
Physiology of wound healing Advanced wound assessment Advanced wound dressing products Wound debridement o Theoretical o Practical Wound infection Complex wound types (leg ulcers, pressure ulcers, diabetic foot ulcers, malignant/fungating tumours) Vascular assessment o Theoretical o Practical Compression bandaging o Theoretical o Practical Complex case studies – 7 – Advanced Wound …
Wound healing is a complex and highly regulated process that can be compromised by both endogenous factors (pathophysiological) and exogenous factors (micro-organisms). Microbial colonisation of both acute and chronic wounds is inevitable, and in most situations endogenous bacteria predominate, many
The use of human skin equivalents has been shown to promote wound healing in diabetic ulcers via the action of cytokines and dermal matrix components that stimulate tissue growth and wound closure. 34,35 A recombinant platelet-derived growth factor is also currently in use and has been shown to stimulate wound healing. 36 However, the present data for most of these modalities are not
Pathophysiology of wound healing Normal wound healing involves a complex and dynamic but superbly orchestrated series of events leading to the repair of …
The literature that exists on the subject of wound healing and tissue repair is vast, and it is soon apparent to anyone who begins to survey it that the majority of studies have been carried out on skin. This of course is not surprising in view of its ready accessibility for experiment and …
Wound-healing model. After 1 week of diabetes induction, the normal and After 1 week of diabetes induction, the normal and diabetic rats were used for wound-healing studies.
the pathophysiology of chronic wounds and rationale for wound bed preparation with negative-pressure therapy dr.ehren eksteen , prof pf coetzee
Wound healing can be delayed by systemic factors that bear little or no direct relation to the location of the wound itself. These include age, body type, chronic disease, immunosuppression, nutritional status, radiation therapy, and vascular insufficiencies.
HISTORY OF WOUND HEALING • Wood Johnson(1876): – Antiseptic dressing (cotton gauze impregnated with iodoform). • The 1960s and 1970s: – Developing of polymeric dressing
Physiology and Pathophysiology of Wound Healing in
Pathophysiology of Morbid Obesity Conference Innovators
Abstract. Wound healing is a complex process that can be divided into at least 3 continuous and overlapping processes: an inflammatory reaction, a proliferative process leading to tissue restoration, and, eventually, tissue remodeling.
• A review of 32 abdominal wound dehiscences in a five-year period shows an incidence of 0.51%. Important factors are preexisting pulmonary disease, “malnutrition,” intraoperative contamination (often minimal), gastrointestinal distention, and aggressive tracheobronchial toilet in the postoperative period.
A reliable method of determining wound healing rate D. Cukjati S. Rebersˇek D. Miklavcˇicˇ Faculty of Electrical Engineering, University of Ljubljana, Ljubljana, Slovenia Abstract—Several wound healing rate measures have been introduced with the main goal of enabling quantification of the effects of various therapeutic modalities on the healing of open wounds. Different definitions of
Wound healing is a complex process of repairing after tissue injury. Burn is one of the most common types of injuries. SSD cream is the gold standard treatment used for preventing bacterial gram positive and gram negative growth in the burn wound and for wound healing.
Impaired wound healing is not an uncommon occurrence in clinical practice. Both local and systemic factors are responsible for impaired healing and weak scar tissue formation. Acute wounds heal following the normal sequence of the healing process.
Wound healing and diabetes mellitus David G. Greenhalgh, MDa,b,* aShriners Hospitals for Children Northern California, 2425 Stockton Boulevard, Sacramento, CA 95817, USA bDepartment of Surgery, University of California at Davis, 2730 Stockton Boulevard, Sacramento, CA 95817, USA One of the leading causes of impaired wound healing is diabetes mellitus. Unlike other causes of altered tissue
pdf PDF Plus There has been a great deal of research into the ways in which drugs affect the physiology of wound healing, but to understand it the nurse must know what the normal processes are.
Venous leg ulcer (VLU) is one of the most common lower extremity ulcerated wound, and is a significant healthcare problem with implications that affect social, economic, and the well-being of a patient. VLU can have debilitating related problems which require weekly medical care and may take months to years to heal. The pathophysiology of VLU
Burn Pathophysiology Jackson’s Burn Wound Model is a model for understanding the pathophysiology of a burn wound that has been often described in the literature( 4-10 ). The zone of coagulation nearest the heat source is the primary injury.
Wound healing is a complex and highly regulated process that can be compromised by both endogenous factors (pathophysiological) and exogenous factors (micro-organisms). Microbial colonisation of both acute and chronic wounds is inevitable, and in most situations endogenous bacteria predominate, many
ABSTRACT: This is the second of 2 articles that discuss the biology and pathophysiology of wound healing, reviewing the role that growth factors play in this process and describing the current methods for growth factor delivery into the wound bed
the pathophysiology of chronic wounds and rationale for wound bed preparation with negative-pressure therapy dr.ehren eksteen , prof pf coetzee
Impaired wound healing is a frequent and very severe problem in patients with diabetes mellitus, yet little is known about the underlying pathomechanisms. In this paper we review the biology of wound healing with particular attention to the pathophysiology of chronic wounds in diabetic patients. The standard treatment of diabetic ulcers
Pathophysiology exam questions Semmelweis Egyetem
Pathophysiology of acute wound healing ScienceDirect
This review will cover some important aspects of general wound healing, and then discuss the important aspect of the pathophysiology of wound healing in VLU, differentiate VLU that heal versus VLU that are classified as non-healing with respect to the biochemical properties of the wound.
pathophysiology of burns . Major thermal injuries are accompanied by marked pathophysiological and immunological changes. These have been extensively detailed by Arturson (1985 pp.129-146) and Britto et al (1999 pp.103-112).
Pathophysiology of Morbid Obesity Tony Burn Alfred Hospital, Melbourne, Australia Introduction Obesity is an epidemic disease which is increasing in frequency in Australia
Clinics in Dermatology (2007) 25, 9 – 18. Pathophysiology of acute wound healing Jie Li, PhD*, Juan Chen, MD, Robert Kirsner, PhD Department of Dermatology and Cutaneous Surgery, University of Miami Miller School of Medicine, Miami, FL 33136, USA
Wound healing is a complex and highly regulated process that can be compromised by both endogenous factors (pathophysiological) and exogenous factors (micro-organisms). Microbial colonisation of both acute and chronic wounds is inevitable, and in most situations endogenous bacteria predominate, many
The initiation of healing starts with the creation of a wound. A wound is defined as an injury to the body that typically involves laceration or breaking of a membrane and damage to the underlying tissues.1 Injury can occur from any number of mechanical or thermal forces that lead to disruption of the skin and damage to the connective tissue and vasculature. Bleeding ensues along with exposure
Impaired wound healing is a frequent and very severe problem in patients with diabetes mellitus, yet little is known about the underlying pathomechanisms. In this paper we review the biology of wound healing with particular attention to the pathophysiology of chronic wounds in diabetic patients. The standard treatment of diabetic ulcers
The literature that exists on the subject of wound healing and tissue repair is vast, and it is soon apparent to anyone who begins to survey it that the majority of studies have been carried out on skin. This of course is not surprising in view of its ready accessibility for experiment and …
Wound healing is a complex process of repairing after tissue injury. Burn is one of the most common types of injuries. SSD cream is the gold standard treatment used for preventing bacterial gram positive and gram negative growth in the burn wound and for wound healing.
Clinical Practice Guidelines. In 2003, the Wound Healing Foundation (WHF) and president Dr. Elof Eriksson determined that standards based on evidence should be developed specific for wound healing.
A reliable method of determining wound healing rate D. Cukjati S. Rebersˇek D. Miklavcˇicˇ Faculty of Electrical Engineering, University of Ljubljana, Ljubljana, Slovenia Abstract—Several wound healing rate measures have been introduced with the main goal of enabling quantification of the effects of various therapeutic modalities on the healing of open wounds. Different definitions of
• A review of 32 abdominal wound dehiscences in a five-year period shows an incidence of 0.51%. Important factors are preexisting pulmonary disease, “malnutrition,” intraoperative contamination (often minimal), gastrointestinal distention, and aggressive tracheobronchial toilet in the postoperative period.
Physiology of wound healing Advanced wound assessment Advanced wound dressing products Wound debridement o Theoretical o Practical Wound infection Complex wound types (leg ulcers, pressure ulcers, diabetic foot ulcers, malignant/fungating tumours) Vascular assessment o Theoretical o Practical Compression bandaging o Theoretical o Practical Complex case studies – 7 – Advanced Wound …
How Diabetes Affects Wound Healing. Tweet. Diabetes is a condition in which the body does not effectively use sugar. It is estimated that there are nearly 18 million Americans with diabetes, and approximately 15 percent of diabetics will develop a foot ulcer at some point. Foot ulcers are the most common wounds for this patient population. Wound healing can be slowed when the patient is
Wound classification and the basic principles of wound healing are reviewed here. The factors responsible for impaired wound healing and wound complications, as well as the clinical assessment and management of wounds, are reviewed elsewhere. (See
Diabetes and Wound Healing Pathophysiology Regulating
Acute and Impaired Wound Healing Pathophysiology and
pathophysiology of burns . Major thermal injuries are accompanied by marked pathophysiological and immunological changes. These have been extensively detailed by Arturson (1985 pp.129-146) and Britto et al (1999 pp.103-112).
Wound healing and diabetes mellitus Semantic Scholar
Current Aspects in the Pathophysiology and Treatment of
This is the first installment of 2 articles that discuss the biology and pathophysiology of wound healing, review the role that growth factors play in this process, and describe current ways of growth factor delivery into the wound bed.
Cutaneous scarring Pathophysiology molecular mechanisms
Pathophysiology exam questions Semmelweis Egyetem
NON-INVASIVE ASSESSMENT OF WOUND-HEALING PATHOPHYSIOLOGY