Biopsychosocial model of pain pdf
Introducing the Biopsychosocial approach as the model for good medicine and good doctors. Development of a new model. Until recent decades the traditional approach towards health and
relevant to return to work for those with poor mental health. In a systematic review of literature, Blank and colleagues (2008) In a systematic review of literature, Blank and colleagues (2008) identified that the medical condition was a factor in return to work.
The BioPsychoSocial Model of Pain The medical model has been very successful in treating a wide range of diseases and conditions. The idea of enquiring after symptoms, looking for signs, getting investigations, making a
chronic pain is, how pain signals are transmitted in the body, the role of the brain in processing pain information, and an explanation of the biopsychosocial model of pain and the transactional
known as the biopsychosocial model, with pain viewed as a dynamic interaction among and within the biological, psychological and social factors unique to each individual. Indeed, as reported by Gatchel 4, Figure 1 presents a conceptual model of these interactive processes involved in health and illness. Pain is not purely a perceptual phenomenon in that the initial injury that has caused the
Pain is now appreciated from the biopsychosocial perspective, as is human health and functioning in general, and is considered part of evidence-based ‘best practice’. The biopsychosocial model in general is congruent with osteopathic philosophy and provides a wealth of evidence which underpins the osteopathic approach.
The Psychology of Pain within the Biological Model Michael Coupland, CPsych, CRC Integrated Medical Case Solutions (IMCS Group) Integrated Medical Case Solutions National Panel of Psychologists • Biopsychosocial Pain Evaluations • Functional Psychological Evaluations • Opioid Assessment and Intervention • Early Identification of Chronic Pain and Delayed Recovery Michael …
Through biopsychosocial model, empirical research about rheumatoid arthritis highlights the interdependence among psychological factors (cognitive, behavioural and emotional ones), psychopatological outcomes (measured as anxiety and depression), physical outcomes (showed by self-reported pain and disability) and physiological ones (measured by
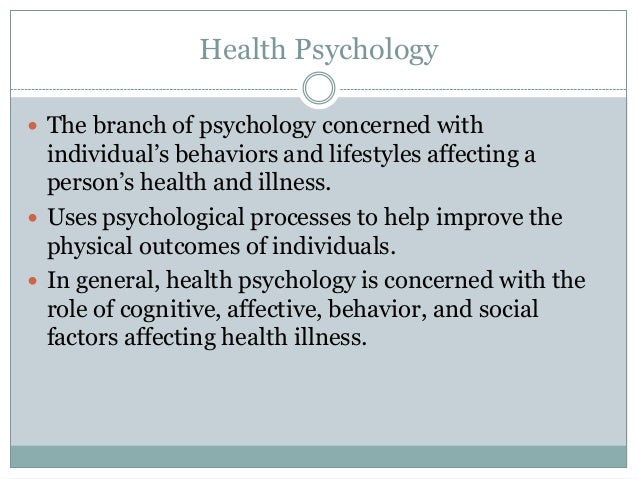
The biopsychosocial model served as incentive for many studies of how psychological and social factors influence the development, course and outcome of a …
As pain involves multiple body systems and affects the whole person, it is best managed with an holistic biopsychosocial model of treatment rather than with a purely biomedical (local tissue damaged) model.
”Chronic pain is a biopsychosocial condition that often requires integrated, multi-modal, and interdisciplinary treatment, all components of which should be evidence-
period (60–66%). When the medication needed adjustment, this commonly consisted of an increase in the dose of the current medication or addition of another medication
The biopsychosocial model of lower back pain – find out how your thoughts and beliefs affect your pain. Bio-Psychosocial Model of Back Pain If you are trying to get control of your back pain there are five important things to consider:
Assessment of Biopsychosocial Risk Factors for Medical
https://youtube.com/watch?v=7mKU0ipLwsQ
(PDF) The Biopsychosocial Model of the Assessment
BIOPSYCHOSOCIAL MODEL OF HYPNOSIS 35 A growing body of research supports the efficacy of hypnosis and hyp-notic treatments for benefiting individuals with a variety of conditions
This approach to pain, which takes into account a number of different factors, is known as the biopsychosocial model of pain. ‘Model’ means the viewpoint taken by those treating your pain. ‘Model’ means the viewpoint taken by those treating your pain.
What exactly is a biopsychosocial approach to health? The biopsychosocial approach includes four primary components that need to be addressed when maintaining health. For more information on how to The biopsychosocial approach includes four primary components that need to be addressed when maintaining health.
A biopsychosocial model of low back pain and disability. ICF, International ICF, International Classifications of Functioning, Disability and Health: WHO, World Health
of care in persistent orofacial pain. The biopsychosocial model of care was first introduced to the medical literature in the late 1970s (Engel 1977, 1980, 1985) in order to acknowledge that there is more to a disease or a disorder than just its biomedical aspects. The biopsychosocial model acknowledges that any disease or disorder is a biopsychosocial entity; that is, it has biological
Pain is one of the primary reasons to seek care, and a greater understanding of pain within the biopsychosocial model potentially widens the scope of the osteopathic consultation to consider the broader consequences of acute or chronic pain on the overall health of the patient, and open up more diverse options for intervention than simply ‘hands on’.
Basically, the biopsychosocial model takes into account the dynamic interactions among bio, psycho and social factors in the pain-experience process. 5,8 However, in order to continue to provide effective pain management approaches, the model must adapt as our knowledge and technology advances.
However, the results of the national survey on pain psychology suggest that while medical providers may recognize the value of the biopsychosocial model of pain treatment, they appear to be lacking the resources to operationalize this model in their practices .
The biopsychosocial model basically means addressing the problem of chronic pain in three ways: bio=any biological considerations ie injury or illness psycho=how you think and feel about the problem
consider the biopsychosocial model, which views physi- cal illnesses as the result of the dynamic interaction among biological, psychological, and social factors [3]. Poor biopsychosocial functioning has been found to pre-dict higher pain severity in CLBP patients [4]. Biological functioning refers to general physical functioning and the extent to which health limits physical activities. This

attachment style and chronic pain syndrome: the importance of psychological and social variables in the biopsychosocial model of chronic pain
The biopsychosocial model has been demonstrated to be the most heuristic approach to chronic pain assessment, prevention, and treatment. Currently, this model also provides the best foundation for
Biopsychosocial model has failed to provide ‘a blueprint for research…and a design for action’. Reductionism as a concept, on the other hand, has undergone further refinements in contemporary theories of philosophy and proved to be practically useful, generate testifiable data and valuable asa research tool for biological sciences.

Validation and Clinical Application of a Biopsychosocial Model of Pain Intensity and Functional Disability in Patients with a Pediatric Chronic Pain Condition
A History of Biopsychosocial Pain 2 to intensity for hundreds of years. It could, therefore, be argued that the biopsychosocial model of pain has been evident throughout history and
The following outline compares the presentation, diagnosis, and treatment used by physicians who follow the biomedical and biopsychosocial model: Biomedical Model Reason for visit: Patient complains of chest pain.
From the Acute Pain to the Biopsychosocial Model. Patients should be encouraged to contribute to their own treatment plan, but they should also be guided towards an acceptance of the biopsychosocial model.
134 E. Atkins et al. ill babies and children providing a high level of observation and intensive medical care. PICU admission can have a large psychological effect
Assessment of Biopsychosocial Risk Factors for Medical Treatment: A Collaborative Approach Daniel Bruns Æ John Mark Disorbio The Author(s) 2009.
BARRIERS TO RETURN TO WORK Comcare
Understand the biopsychosocial model of pain Better understand why acute and chronic pain should be treated differently Understand common treatment options
The management of chronic pain centres on improving quality of life through reactivation. The Pain Clinic offers a number of interventions and programmes to help patients take control of their pain:
Engel’s biopsychosocial model10 is rightly considered a landmark contribution to the pain field. The dominant application of the biopsychosocial model has been, and to a large extent remains, focused on the impact of pain on sufferers and those around them. The impor-tance of psychosocial factors as mediators of suffering has been well recognized, and several effective
A biopsychosocial model of low back pain and disability. ICF, International Classifications of Functioning, Disability and Health: WHO, World Health Organization. (refer to Waddell (2004)) 5. Implementing a biopsychosocial approach A biopsychosocial approach to injury management that provides programs tailored to the individual’s needs has the best chance of maximising recovery and …
A biopsychosocial approach to Pain management . Biological, psychological, and social factors interact to impact the experience of pain. The interaction among these factors is called a “biopsychosocial model”.
The National Institute for Health and Clinical Excellence has called for greater use of the biopsychosocial model to manage patients with low back pain (LBP) alongside early detection and treatment of symptoms.
The Biopsychosocial Model of the Assessment Prevention
The authors describe a biopsychosocial model of chronic pain and provide an update on research implicating the importance of people’s appraisals of their symptoms, their ability to self-manage pain and related problems, and their fears about pain and
The biopsychosocial model further accounts for the bidirectional influences of the biological, psychological, and social aspects of pain with, for example, psychological factors influencing biology by changing the production of hormones (e.g., cortisol), and brain structures and processes (Turk & …
A biopsychosocial approach to chronic low back pain and disability in a private chiropractic setting: a case study Kevin A. Parish, BSc, DC, FCCRS(C)* For the clinician in private practice, a patient presenting with chronic low back disability can be challenging. Physical factors as well as psychosocial factors play a role in the development of chronicity. In fact, psychosocial factors may be
Pain is one of the most common reasons for entry into the primary health care system which includes seeking care from osteopaths, primarily for musculoskeletal pain.Pain is now appreciated from the biopsychosocial perspective, as is human health and functioning in general, and is considered part of evidence-based ‘best practice’.The biopsychosocial model in general is congruent with
The biopsychosocial model has led to the development of the most therapeutic and cost-effective interdisciplinary pain management programs and makes it far more likely for the chronic pain patient to regain function and experience vast improvements in quality of life.
biopsychosocial (BPS) model Practical Pain Management
The BioPsychoSocial Model of Pain The Physiotherapy Site
BIOPSYCHOSOCIAL MODEL • “The dominant model of disease today is biomedical, and it leaves no room within its framework for the social, psychological, and
Objective. To cross-validate a biopsychosocial model using physical disability, helplessness and passive coping to predict depression and pain in rheumatoid arthritis (RA). Methods. Clinical and psychological measures were collected from 157 RA patients at three time points over a period of 12
The flags model has been used to describe psychosocial prognostic factors for the development of persistent pain and work disability following the onset of musculoskeletal conditions. It is widely acknowledged that a biopsychosocial approach to managing compensable musculoskeletal injuries can lead to better health outcomes.
Contemporary knowledge and thinking advocates an integrated biopsychosocial model for the more effective management of spino-pelvic pain disorders. However, the ‘bio’ aspect seems to be the poor relation to the psychosocial at the moment.
Chronic back pain is a leading cause of disability that has a major impact on patients, doctors, healthcare systems, and workplaces. 1 Despite growing use in some countries of spinal imaging, opioid analgesics, spinal injections, and spinal fusion surgery, disability from back pain has increased. 2
it is a pragmatic application of the biopsychosocial model of pain, but differentiating it from cognitive behavioural therapy and educational components of early multidisciplinary pain management programs.
model is now widely accepted as the most heuristic approach to chronic pain. With this model in mind, With this model in mind, a review of the basic neuroscience processes of pain (the bio part of biopsychosocial), as well as the
Unlike the biopsychosocial model, this model is more than a collection of data points. It is a formulation—a hypothesis about why this patient has fallen ill now. Emphasis on development draws attention to underlying vulnerabilities and diatheses on which present stressors operate to create a theory of causation that integrates genetic and environmental effects, and suggests a treatment plan
Biopsychosocial Model of Chronic Pain Dr. John Otis

Biopsychosocial care and the physiotherapy encounter
founded on research related to the biopsychosocial view of pain. The services and programs provided at hospitals in NSW appear to vary based on the local context and history of the service.
4/27/2016 1 Bio-psycho-social Model of Pain: A Shifting Philosophy Judith Scheman, Ph.D. Cleveland Clinic Center for Neurological Restoration
BioPsychoSocial model of pain Health Psych
Biopsychosociale model of pain « University Pain Centre
Bio-psychosocial model of pain Pain Clinic (The onion
[The biopsychosocial model of adjustment of the rheumatoid
Bio-psycho-social Model of Pain A Shifting Philosophy
Pain Psychology and the Biopsychosocial Model of Pain